Racism and Health
It’s time the country came to terms with the fact that racism impacts health.
That’s the growing call of a number of local governments and health organizations across the country. Three states and more than 50 municipalities have made these declarations, and in September the Anti-Racism in Public Health Act was introduced in the U.S. Senate, a bill that would create organizations within the Centers for Disease Control and Prevention (CDC) to research anti-racist health policies and focus on prevention of law enforcement violence and brutality.
Decades of research have shown that race is a predictor of health outcomes.
Native Americans, blacks and Hispanics are over four times more likely than white people to be hospitalized with COVID-19.
Hand-washing is key to reducing the spread of COVID-19, but some Indian tribes have no access to running water.
For people in the public health sector, these actions and legislation are a long time coming. Decades of research have shown that race, separated from other factors like income and education, is a predictor of health outcomes. Yet for much of the population, it has taken police brutality and a global pandemic to recognize that racism impacts economics and health to a dramatic extent.
Racism, according to the American Public Health Association, is very much tied to both economics and health. Race is a way to assign value and opportunities, making some people advantaged and others unduly burdened.
“Race manifests really specifically in the way we organize our value systems and resource allocations,” says Paula Tran Inzeo, director of the Mobilizing Action Toward Community Health program at the University of Wisconsin-Madison Population Health Institute. “Structural racism can create opportunities for some and disadvantages for others in communities. In the United States, we have created patterns of disadvantage for blacks and other people of color.”
Shining a Light
As data on COVID-19 began to flow in and be analyzed, it quickly became apparent who was most at risk if infected with the new coronavirus. According to the CDC, when compared to white people, Native Americans, blacks and Hispanics are at least 2.6 times more likely to catch the virus and more than four times more likely to be hospitalized with it, and blacks are more than twice as likely to die from COVID-19.
This is particularly true in larger cities, where there are higher concentrations of people of color. Black residents of Washington, D.C., for example, are almost six times more likely to die than white residents. Black people also have had higher death rates from COVID-19 in Chicago, St. Louis, Milwaukee, New Orleans and Detroit.
Another report by Pew Charitable Trusts found that in states with the highest percentage of blacks, “the prevalence of death among black residents exceeded their population share by as much as 25 percentage points.”
In Massachusetts, which had one of the highest infection rates in the nation, researchers culled data to determine how the virus was affecting minority populations in the state. They found that an increase in black and Hispanic populations in a town was associated with a much higher number of cases. The city of Chelsea, where minorities make up a majority of residents, had the highest infection rate, almost six times higher than the state’s average.
“While we know we are all at risk, what we have seen is who gets sickest and dies is disproportionately black and indigenous people of color,” says Tia Taylor Williams, director of the Center for Public Health Policy and the Center for School, Health and Education at the American Public Health Association. “We need to come together to elevate that need and start acting on racism as a driving force that impacts factors like health and life outcomes.”
Why the Disparity?
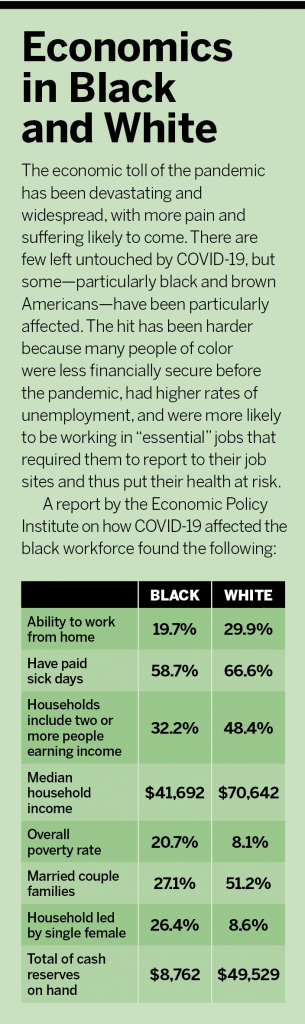
COVID-19 appears to hit blacks and others of color hardest not because they are more susceptible to this particular illness but because the virus exacerbates pre-existing inequities in health and economics. Some chronic conditions that can cause worse outcomes for people with COVID-19 are found in much greater numbers in black and Hispanic populations. According to the Economic Policy Institute, black Americans are 1% more likely to have asthma than whites, over 6% more likely to have diabetes, 12% more likely to have hypertension, and 7% more likely to be obese.
“Chronic disease rates are higher among people of color, and we have to ask why,” Williams says. “There is some genetic predisposition for hypertension, but there’s nothing inherent about being black that puts you at a higher risk for obesity.”
Being more likely to have good health outcomes, she says, often depends on larger structural factors that can be driven by racial discrimination. These include clean housing, living in neighborhoods that are safe to walk or exercise in, and nearby, affordable access to healthy food.
“A driving force is the social determinants of health,” Williams says. “It’s taking different topics that influence health and trying to look at how racism affects them and how resources for those things are allocated and distributed.”
For instance, good hand-washing practices are a major component of reducing the spread of COVID-19. But she found that some Indian tribes have no access to running water. White communities, she says, received COVID-19 testing earlier than others, but when it was available in minority communities via drive-throughs, people needed cars to get to the testing sites.
Wisconsin, whose minority populations have had inferior health outcomes, has been working for years to right the scales. The state has continued to do poorly, though, says Inzeo, because groups haven’t been effectively addressing those root causes. A 2019 report from the Wisconsin Collaborative for Health Care Quality found that black children in the state are less likely than white children to be vaccinated, maintain a healthy weight, and have controlled blood pressure.
Inzeo says Wisconsin residents still suffer from redlining, noting that blacks in the state don’t have full access to home ownership because of years of racist lending practices. “It continues to persist today—systems of the wealth creation that advantaged some and left others behind,” Inzeo says.
With public education funding based on property values, Inzeo says, many black, Hispanic and indigenous families have less optimal schools in lower-income communities where mass incarceration is much more common. In most studies looking at social determinants that contribute to poor health outcomes, education tops the charts. For instance, in the United States, life expectancy rates are lower among people without a high school education and improving among people with high school diplomas.
Indigenous people also had low vaccination rates and were less likely than whites to have breast cancer screenings. Both groups also tended to continue tobacco use, even if they have diabetes or heart disease. Studies have shown that low-income communities and more blue-collar businesses are less likely to implement cessation practices like smoke-free community spaces and workplaces.
Even when the intentions were good in Wisconsin—the state has been progressive in its Medicaid expansion—inequities can persist.
“Access to insurance is only as good as the access to a provider with quality care that you can get to,” Inzeo says. “In rural communities, there are problems with accessing providers because of transportation or lack of the kind of care people might need. Insurance access is incredibly important, but it requires thoughtful implementation.”
Specific structural racism factors hit black, Hispanic and indigenous populations particularly hard during the pandemic. These populations are more likely to be essential workers, meaning they are not as likely to be able to work from home. They also more commonly live in urban areas with larger household sizes and are more frequent users of public transportation. All of these things put people at higher risk for contracting COVID-19.
Economically, the pandemic took a greater toll on people of color as well. Not only does that add stress, but it can also diminish one’s ability to pay for healthcare when they may need it most. According to a Health Affairs study, less than half of the U.S. Hispanic workforce has paid sick leave.
Food services, retail, and healthcare—all essential industries—had the highest number of layoffs in April, according to the U.S. Bureau of Labor Statistics. Among all black-owned businesses, 27% fall within these sectors. By comparison, among all white-owned businesses, only 19% are in food services, retail, and healthcare.
While blacks had much higher unemployment rates, those who continued to work during the virus-induced lockdown earlier this year were disproportionately exposed to COVID-19 in the workplace. Although blacks make up about 12% of the workforce, they account for 17% of front-line industry workers—14% of grocery workers, 26% of public transit workers, 17% of healthcare workers and 19% of social service workers.
According to a September report from The Commonwealth Fund, 31% of black people and 26% of Hispanics have been unable to pay for necessities like rent and food during the pandemic. That compares to 10% of white Americans. Another 38% of blacks and 49% of Hispanics have used all or most of their savings to get through the pandemic, whereas only 15% of whites reported doing so. And more than twice as many black and Hispanic Americans also reported borrowing money, taking out loans and suffering economic hardship during the pandemic than whites.
Making a Change
A majority of the efforts to declare racism a public health issue have come from the local level. This is likely because the issue is so politically charged. But it also may be because it is such a localized issue. Policing is funded and impactful to those within its purview. Health systems deal with patients in their treatment areas.
“People are trying to concentrate their efforts on the distribution of resources at the county and local level,” Williams says.
Three years ago, Inzeo says, when public health groups in Wisconsin began to talk about the impact of race on health, the subject was not nearly as well received as it is today. Her organization created a sign-on for its website, stating that “Racism is a Public Health Crisis.” When groups sign the online declaration, they commit to taking action. More than 150 organizations have signed up, including Milwaukee County, which now takes into account racial equality when creating its strategic plan and making policing and budget decisions. The county Facilities Administration created a human resources program manager for diversity and inclusion. And, in spite of a budget shortfall in 2020, the county maintained its public transit system without raising fares, crucial for underserved communities.
Employers may feel like public health and racism aren’t issues that touch their employees or communities. Whether they are present within an organization, employers would be remiss to let this flashpoint pass without understanding how they may be able to make a difference.
“Being dismayed at what is happening or making the statement that black lives matter is not sufficient,” says Kira Hudson Banks, a principal at the diversity training firm The Mouse and The Elephant. “We need action. I think every organization has a way that they can engage in this work either directly or simply by understanding if, within the walls of their organization, they are creating opportunities for all workers.”
Williams recommends every business start by looking internally. When thinking about racism and public health, issues like economics and healthcare access are high on the list of challenges. Employers can look at their workforce, their trustees and other decision makers and see if they look alike. Does the C-suite look like the rest of the organization and the community it serves? If not, businesses can do some soul searching to find out why—and then start bringing different people to the table.
“Are we allowing people to be their full selves and live to their full potential, or is that disproportionately accessible only to white people?” Banks says.
Too often, she says, organizations unintentionally create environments in which only white men thrive. This is often blamed on a pipeline that lacks diversity, but Banks says more subtle aspects are usually at play. Companies are often more likely to mentor white employees and offer assignments that make them stretch and grow, which leads to upward mobility, Banks says, while telling people of color they need to develop and grow before they can have those same opportunities.
Employers should also understand that, as younger generations move into the workforce, they will likely be less tolerant of racism at work.
“Young people of color were not from the movement of the sixties that were happy just to be let in the door,” Banks says. “We raised them in a society that told them we were post-racial and color blind, and they feel lied to. What we told them is different than what they are experiencing. They will be in the corporate space in a few short years, and it appears they are less tolerant of an unequal society.”
For employers who feel like their organization is on track, Banks suggests running data to prove it. Look at employee satisfaction, recruitment, engagement or impact of services in the community through the lens of race and gender. Businesses can determine relatively quickly if they are equitable that way. If a company is not, she says, organizations have to be willing to “call out those skeletons in the closet rather than waiting for someone to call them out. Be proactive and control the narrative.”
Along with working to improve diversity among management, employers can ensure employees have living wages and that pay inequities that appear to be related to things other than performance are addressed.
Insurance and Access
One critical space where companies can work to improve employees’ economics and health is through equitable insurance offerings. A report released in August by The Geneva Association noted that income inequality in lower- to middle-income countries has a direct relationship with “ineffective” insurance. This includes slim health insurance plans that put patients at risk of paying for too much out of their own pockets or forgoing treatments because of their inability to pay.
Employers can look within their own ranks to make sure deductibles aren’t too high for their low-wage workers. Businesses can ensure that people of color aren’t disproportionately among the ranks of people working part-time and ineligible for health insurance. Employers can also offer and promote products such as life insurance to all employees. A University of Michigan study found that, after the death of a spouse, 33% of secondary earners without life insurance were at risk for financial hardship. Among those who did have life insurance, that number dropped to 24%.
Sarah Klein, a consulting writer and editor at the Commonwealth Fund, says employers can also affect quality healthcare access for everyone within a company and a community.
“If an employer said, ‘I want to see evidence that all employees are being treated equally …. I want to see that screening rates for colorectal cancer are equivalent for everyone, and you need to prove it,’ insurers are very responsive,” Klein says. “Employers don’t know the power they have over insurers.”
There hasn’t been a big move to collect racial or ethnic data that would allow for quality healthcare measurements broken down in those areas, Klein says. But if enough employers say it’s a priority, insurers will listen. And when insurers seek these details, they force healthcare providers to track them more frequently. This can also make providers more aware of their numbers and improve the overall health of a community.
Ensuring equitable access to care can also reduce costs for employers. The North Dakota Department of Health looked at the issue and found that, from 2003 to 2006, eliminating disparities for minorities would have reduced direct health costs by $229.4 billion nationwide. During that time, the department found, 30% of direct medical costs for minorities were excessive costs caused by unequal care.
Now is the time for employers to look at their organizations and find out if everyone is being treated equally at all levels and through all programs, including benefits. Banks says racism and its impact on health isn’t a problem that we can “hope our way out of.” The antidote to racism isn’t to say people don’t see race or color. Rather, she says, it’s time to see race more clearly and pinpoint exactly where it is being used to create access or inequity.
“It’s about seeing how racism has attributed to how we do life,” she says. “And if we have created inequalities, can we create a space where they no longer exist?”
Banks likens making these changes to wearing seatbelts. In the 1960s and 1970s, people drove cars without much thought to wearing the belts. Drivers couldn’t be counted on to wear restraints, even though it could save their lives. When it became clear that people fared better after crashes when they wore seatbelts, systems were put in place to force the issue, and laws were passed requiring people to wear seatbelts.
“It wasn’t popular to make people wear seatbelts,” Banks says. “But now we are accustomed to it.
“It’s not about everyone understanding—we are not going to hold our breath for everyone to do that—but there are enough people who do get that this is an issue to make it work. Employers need to come up with solutions, like the ding in our seatbelt, where we are acting more equitable and there are disincentives not to act that way.”