Advantage, Medicare
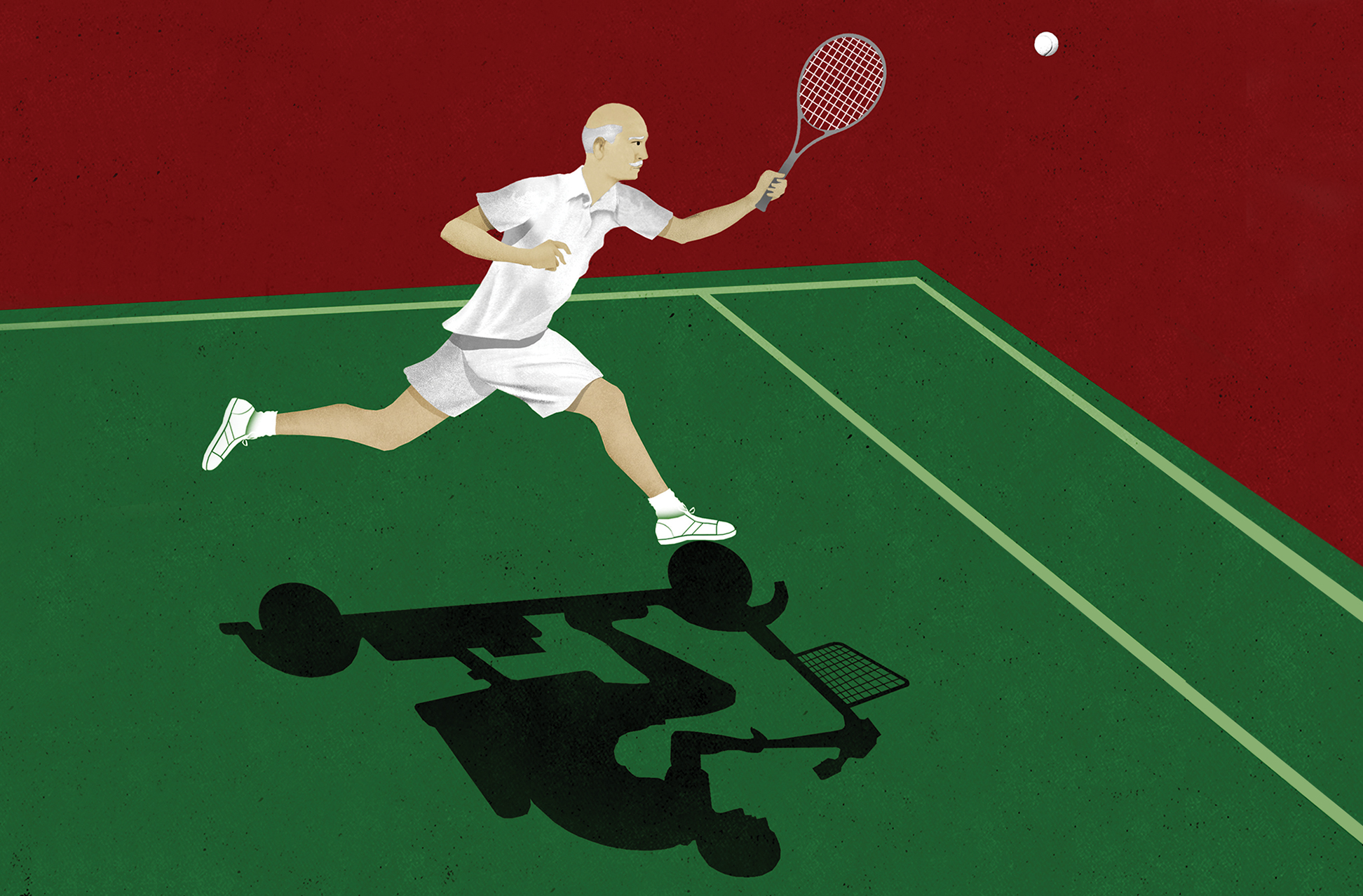
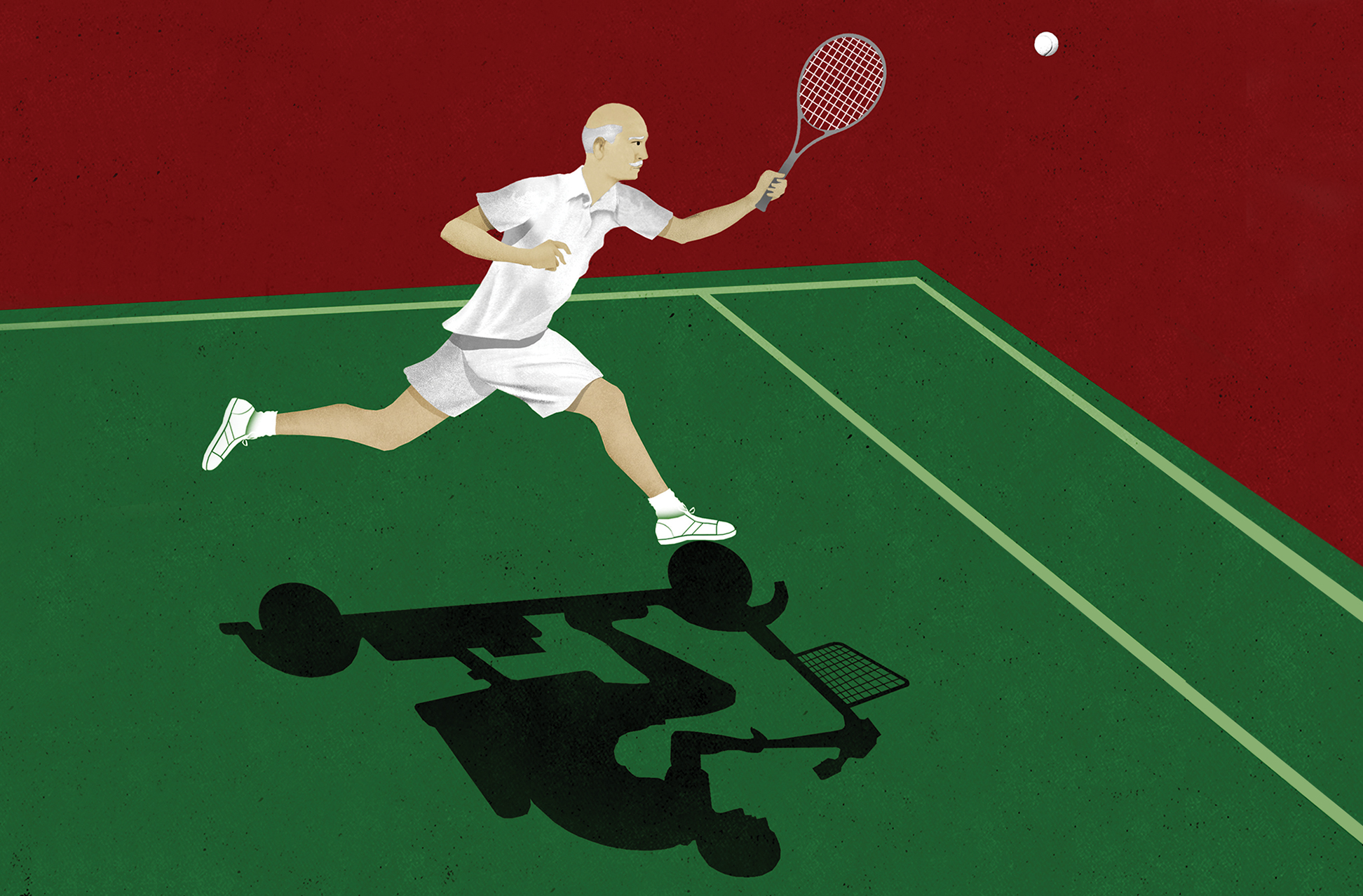
Millions of baby boomers entering retirement each year are faced with a vast, complex ecosystem of health insurance plans that begs someone—an expert, preferably—to advise boomers of their options.
One such choice is Medicare Advantage, and it’s making waves. Medicare Advantage plans are private insurer alternatives to traditional Medicare health insurance coverage. These plans are an interesting trade-off, offering lower prices and unique care-coordination services, such as extra rides to appointments, private home health aides, and home-delivered meals, but at the expense of wide provider networks, among other things.
In 2019, 22 million people, about one third of all Medicare beneficiaries, were enrolled in Medicare Advantage plans.
The Congressional Budget Office projects the share of Medicare beneficiaries in Medicare Advantage plans will rise to about 47% by 2029.
Medicare Advantage offers lower prices and unique services but lacks wide provider networks.
In 2019, 22 million people, about one third of all Medicare beneficiaries, were enrolled in Medicare Advantage plans, similar to the proportion in 2017 and 2018, according to the nonprofit Kaiser Family Foundation. The growth in total Medicare Advantage enrollment has been steady at around 8% for the past three years. But the Congressional Budget Office projects the share of Medicare beneficiaries enrolled in Medicare Advantage plans will rise to about 47% by 2029, Kaiser reports.
The expected growth of Medicare Advantage reflects a general move toward a more thoughtful and comprehensive approach to senior medical care, says Allyson Schwartz, president and CEO of the Better Medicare Alliance, a national research and advocacy group supporting Medicare Advantage that includes 143 organizations representing healthcare providers, plans, patient organizations and community groups.
“Healthcare providers now better understand the role of care coordination in integrated systems of care, including primary care and having care teams available to seniors,” Schwartz says. “This reflects not only greater and more flexible clinical engagement, such as being proactive in monitoring seniors’ health and demonstrating flexibility through the use of innovations such as telemedicine, but also a greater understanding of the broader health issues that seniors and those with disabilities face, such as can they get to the doctor’s office, do they need post-hospital care help at home, and do they need meal support. Medicare Advantage’s popularity also reflects the popularity of benefits like dental, hearing and vision care.”
“Medicare Advantage plans are the fastest-growing segment of the Medicare population,” notes Matthew Miklos, vice president of Individual Medicare Solutions at InsureOne Benefits, a family-owned insurance brokerage that was acquired last fall by Oswald Companies. Oswald made the purchase in large part to enable the expansion of InsureOne’s senior-products lines on a national basis. “Our primary focus is to grow the business in the Medicare market,” Miklos says. “People are aging in daily even though they may work well beyond 65. For brokers and agents, there is a tremendous opportunity in this space.”
Miklos says Medicare Advantage has gained a lot of ground over traditional Medicare and Medicare Supplement plans in recent years, with the percentage of senior clients who chose Medicare Advantage once eligible rising from no more than 10% five years ago to 40% now. “The reason why Medicare Advantage is winning is that it offers extras like dental, vision, transportation, meals and exercise,” Miklos says. “Also, it is an all-in-one package: dental, vision, hospital, drugs. Essentially, your private carrier is managing Medicare for you.”
Barriers to Entry
Such growth notwithstanding, whether it makes sense for brokers and agents not already in the market to offer Medicare Advantage services might not be so straightforward. There are several barriers to entry and profitability.
- Uncle Sam limits the broker commissions for Medicare Advantage plans.
- There are a vast number of plans and health insurance retirement options whose details must be mastered and whose policies must be painstakingly tailored to, and sold to, each individual.
- Competition is strong, including some national and local brokerages that have been specializing in those plans for quite a while and are expanding.
- We are now halfway through the flow of baby boomers turning 65, the magic number at which they become eligible for such plans and when many seniors make their retirement health insurance selections. Getting established in these lines may take years, and the demand for these services may recede as the much smaller Generation X cohort follows them.
The Magic Number and the Options That Await
The rules governing Medicare, Medicare Advantage and their interaction with other forms of healthcare coverage are complicated. To recount the basics, Medicare is the federal senior health insurance program that serves Americans 65 and older that most citizens must pay into before they retire. Traditional Medicare is composed of four parts: Part A covers inpatient hospital care; Part B covers outpatient services ranging from labs to home health to some surgeries and imaging; Part C is Medicare Advantage; and Part D is prescription drug coverage.
Medicare Advantage plans are private senior healthcare plans under which insurers, instead of the federal government, pay claims by replacing traditional fee-for-service Medicare with a managed care service that generally offers care through an HMO, PPO or similar platform. To join Medicare Advantage, one must still be enrolled in both Medicare Parts A and B, pay Part B premiums, and live in the plan’s service area. One must also not suffer from end-stage renal disease, which necessitates enormously expensive kidney dialysis, though beginning in 2021 this limitation will be removed.
Uncle Sam is putting pressure on insurers to contain costs through Medicare Advantage plans. But that pressure is also being applied to brokers and agents, who receive strictly regulated fees.
“Under Medicare Advantage plans, CMS sets the maximum agent commission, typically $510 for the initial year and $255 per year on renewals,” Miklos says.
The declining fee structure, which varies by state or region, is designed to eliminate “what would otherwise be an incentive to place insureds on a plan even though it was not in their best interest,” Miklos says.
While broker and agent commissions under Medicare Advantage are generally limited to federal fee schedules, there is another potential source of revenue for agents offering Medicare Advantage beyond commissions, says Michael Adelberg, a principal at Faegre Drinker Consulting and a former executive at the federal Centers for Medicare and Medicaid Services (CMS), which regulates Medicare Advantage programs.
In its annual Marketing and Communications Guidelines, CMS enables plans to compensate agents and brokers for administrative services outside of commissions, Adelberg says. “Plans can allow agents and brokers to provide administrative services if they are compensated at fair market value,” he says. “For example, if they help onboard a member in the member’s first month on the plan—essentially serving as a concierge—they can be compensated for that over and above their commission.”
And if carriers do allow compensation for such services, what exactly is fair market value? “When I counsel plan clients, I ask what they were compensated for that activity previously. That would be a good starting place,” Adelberg says. “A member services department could use the cost of department staff or a contractor. It is important that you document how you determined a particular level of compensation. The plan is taking a risk if its fees are unsupported by documentation or are excessive.”
A wide variety of Medicare Advantage plans exist and usually operate as a package offering Parts A and B and usually Part D together in one plan. Unlike traditional Medicare under Parts A and B, enrollees must use a local network of providers. A participant must pay a deductible, co-pays and co-insurance up to the plan’s out-of-pocket maximum, notes Danielle Kunkle Roberts, a founding partner at Fort Worth, Texas-based brokerage Boomer Benefits.
Time matters with respect to making Medicare coverage elections. Turning age 65 is a pivotal event, because Medicare has a limited initial enrollment period, with most seniors having a seven-month window surrounding and including the month the person turns 65.
Right now a vast wave of seniors are entering the initial enrollment window. The baby boomer cohort is finishing its last years of employment and entering retirement at a clip of 10,000 per day, according to the Pew Research Center. Born between 1946 and 1964, the first of them turned 65 in 2011, while the last will not reach this milestone until 2029. A May 2019 story in Leader’s Edge, titled “Will You Still Need Me When I’m 64?” covered this trend and its implications in depth.
Medicare Supplements (Medigap)
The 20%-of-care costs that traditional Medicare plans do not cover can result in sticker shock for many seniors with expensive health conditions or who require expensive procedures. To forgo that shock and other out-of-pocket contributions under traditional Medicare, many choose to pay for Medicare Supplement insurance from private carriers, which are also known as Medigap plans. There are 10 Medigap plans—Medicare Supplement Plan A, B, C, D, F, G, K, L, M and N—each of whose coverage is standardized by the federal government. Plan G covers all of the gaps except the Part B deductible, which makes it a very popular plan. Others cover less of the costs, and none of the Medigap plans pay for dental, vision and hearing exams; long-term care; hearing aids; or retail prescription drugs.
There is no medical underwriting if seniors sign up during the initial enrollment period that commences at the Part B effective date and runs for six months thereafter. After this initial enrollment period, however, medical underwriting is required, and many seniors with significant health conditions will likely not qualify. (This is not true in a few states, such as New York, that prohibit subsequent Medigap underwriting or that offer limited open enrollment windows for Medigap in certain circumstances or during limited periods each year.) Medicare Advantage plans cannot be used with Medigap plans. Unlike Medicare Advantage plans, carriers and/or state legislatures, not the federal government, establish broker and agent fees.
Employer Sponsored Insurance
For those turning 65 who are still eligible for coverage under employer group health insurance plans, there are further wrinkles. “For employees or annuitants covered by group plans from employers with 20 or more employees, there is no penalty to wait to enroll in Medicare—you can save on those Part A and B premiums in the meantime,” Roberts says. “Those who work for smaller employers risk unexpected medical spending if they fail to enroll in Part B, because Medicare is the primary payer when you work for an employer with under 20 employees. If you need knee surgery and Medicare Part B typically pays 80% of that cost for you after you have satisfied that deductible, but you only enrolled in Part A, you may be on the hook for that 80%.”
The interaction of traditional Medicare with group health insurance plans for insureds is complex. The degree to which group insurance results in a useful complement to traditional Medicare—or, conversely, an inefficient, costly duplication of it—may depend upon the structure and richness of the group employer plan.
“We want to look at all the numbers for an individual, not just the monthly premium, such as deductibles, max out of pockets, and networks just to name a few,” Miklos says. “We may find an individual is better off enrolling in a Medicare Advantage plan or traditional Medicare based on any number of differences.”
The considerations are a lot less complex from the viewpoint of the employer: moving older employees off group plans and onto Medicare improves the group experience of employers’ plans and can lower costs for employers and remaining employees. “We are a good tool for employers to help manage a group’s risks,” Miklos says. “You can’t force someone to come off the group policy, but you can educate them and be able to advise and potentially show them what rights and options there are.”
Only a small number of employer group health insurance plans allow employees to retain health insurance into retirement. However, for those that do, Schwartz notes that is one area of growth within Medicare Advantage that brokers can seek to support. “Many big businesses are seeking to cover health benefits for retirees in a manner that is affordable and that yields high satisfaction,” Schwartz says. “One way they can do so is to sign up retirees into Medicare Advantage through an employer group waiver plan [EGWP, pronounced “egg whip”]. That has been undertaken by organizations that include Verizon, GM, and John Deere and sometimes reflects union-negotiated benefits.”
Which Is Best?
A Kaiser Family Foundation study found that healthier seniors generally gravitate toward Medicare Advantage. Seniors with greater medical needs often prefer original Medicare and value the comprehensiveness of original Medicare’s wider network of providers. Those in Medicare Advantage, in contrast, must ensure the physicians, hospitals, medicines and other services associated with those conditions are all covered under their plan or face costly unsupported health costs. Medicare Advantage also might not be the best for seniors who plan on moving around a lot after retirement, as the network of providers for most plans is local, notes Roberts.
In addition, seniors must make elections on Medicare Advantage on an annual basis, and coverage and cost structures can change frequently. Thus seniors with less energy and who are less healthy might not wish to have this obligation, notes Roberts.
In total, 3,148 Medicare Advantage plans are available nationwide for individual enrollment in 2020, a 15% increase from 2019 and the largest number of plans ever available, according to a Kaiser Family Foundation study. These numbers exclude employer- or union-sponsored group plans and Special Needs Plans, which are available to select populations only. Similar to prior years, HMOs continue to account for about two thirds of all plans offered in 2020.
UnitedHealthcare and Humana, the two carriers with the most Medicare Advantage enrollees, have large footprints across the country, offering plans in most counties. UnitedHealthcare is offering plans in 60% of counties, Humana is offering plans in 83% of counties, and plans from both are available in more than half of all counties (53%) in 2020, according to Kaiser Family Foundation.
Medicare Advantage continues to be an attractive market for insurers, with 13 firms entering the market for the first time in 2020, collectively accounting for about 7% of the growth in the number of plans available for general enrollment and about 5% of the growth in Special Needs Plans.
Major carriers have touted Medicare Advantage as a growth area in recent earnings reports. Humana, for example, said it expects 270,000 to 330,000 more members to sign up in 2020 for its individual Medicare Advantage plans for those aged 65 and over, representing 7.5% to 9.2% growth over 2019, according to Reuters. Humana and several carriers declined to comment on their plans and Medicare Advantage approaches.
On the other hand, many who initially sign up for Medicare Supplement plans eventually switch to Medicare Advantage due to the former’s high costs. “The rise in Medicare Part B premiums—on average 5% to 7% each year—is driving more people into Medicare Advantage,” says Don Mackos, a former Humana executive who in 2007 founded RetireMEDiQ, an independent health plan advisory service in Dayton, Ohio, that counsels seniors and those approaching retirement. “When you look at the elderly, that rate increase, coupled with a 5% to 7% increase in Medicare Supplement plans, is leading more seniors into Medicare Advantage. Carriers are also becoming more proficient at packaging and underwriting care in a proactive, economic and holistic manner. Some national carriers, such as Aetna, Anthem and Humana, are developing lower-premium PPO plans that include non-medical supplemental benefits. They are also developing Special Needs Plans for the lower income and for those with chronic conditions.”
The increasing appeal of Medicare Advantage also reflects baby boomers’ greater savvy and willingness to shop around, Mackos says. “The boomers are much more accustomed to networks of providers and co-pays than were people just 10 to 15 years ago,” he says. “How our company interacts with 65- to 70-year-olds is very different than for those 75 or older. That is even the case for those offered rich retirement health plans by their former employers, such as is the case in Ohio with teachers in a statewide retirement system. The teachers can buy a rich plan through their retirement system, but we are seeing many of them looking at individual Medicare Advantage plans to see if they can reduce monthly payments and assume some risk. More and more seniors are acting as consumers, which makes the appeal and attractiveness of Medicare Advantage plans greater than ever.”
The choice of what coverage is best is specific to individuals, with spouses often opting for different coverage. “Sometimes the husband doesn’t believe in going to the doctor, is concerned about cost, and wants the gym membership,” says Elizabeth Gavino, founder of brokerage Lewin & Gavino, which is licensed in 25 states and acts as general agent for 50 agents selling insurance coverage for businesses and older adults. “He may want Medicare Advantage. But the wife may have breast cancer in remission and wants access to any doctor that takes Medicare, or her doctor isn’t in the Medicare Advantage directory. If she has the potential of expensive care ahead, she doesn’t want expensive, unpredictable costs or to have to make coverage decisions while under stress. For her, a Medicare Supplement plan might make sense.”
The Hand of Government
The U.S. government is heavily involved in Medicare Advantage plans and generally likes them a lot. Medicare is one of the largest entitlement programs in the federal budget, and as its long-term solvency remains an open question, many on Capitol Hill regard anything that reduces the government’s obligation as a good thing. Medicare Advantage does that by limiting care options and capitating care payments instead of allowing for recovery of fees for services rendered.
The federal government sets the fees that Medicare Advantage plans, agents and brokers can charge; offers a search engine that helps seniors (and brokers and agents) find and compare care options; and rates plans with a star system. In recent years, the federal government has put its thumb on senior healthcare options to favor Medicare Advantage in not-too-subtle ways. For one, it has allowed brokers and agents to market plans more effectively.
“The CMS has marketing and communications guidelines that limit agent and broker activities, which it relaxed in 2018 compared to earlier guidelines issued in 2016,” says Michael Adelberg, a principal at Faegre Drinker Consulting and a former executive at the federal Centers for Medicare & Medicaid Services (CMS), which regulates Medicare Advantage programs. “There used to be more limits on comparing plans or using superlatives to describe a particular plan. The new rules have made it easier to sell Medicare Advantage and to speak freely. For example, under the older guidance you could not say, ‘Plan X is the best plan,’ unless you supported that statement with empirical evidence, such as Medicare.gov’s star rating for the plan. Now the guidelines are vague about superlatives and more consistent with the state guidelines for selling other types of insurance. It is also permissible for providers under the right circumstance to make a referral to a plan marketing department or representative.”
In addition, Adelberg notes, the Bipartisan Budget Act of 2018 and the Trump administration have expanded the range of new non-medical benefits that plans can offer and be compensated for. That has allowed those marketing Medicare Advantage to distinguish the plans from traditional Medicare on the basis of non-medical components, such as meals and transportation, Adelberg says. Other new offerings from Medicare Advantage include home-delivered meals, pest removal, therapeutic massage, home improvements like ramps, wider hallways and doorways, and adult daycare services and in-home assistance.
Existing Client Integration
There are a variety of ways to get started procuring clients. Some brokers who place other lines of insurance or other financial products cross-sell against existing client bases. “We’ve collected data for years, and we reach out to our existing client base and let them know we are there to advise them,” Miklos says. “We can be a concierge for them.”
Miklos says three buckets of individuals seek his assistance. There are those who are turning 65 who have no access to coverage and have to buy a plan, which he says is a large segment. Another segment that is growing in size includes those working beyond 65 and then retiring at 67 or 69, who need care then. A third group is those who continue to work and prefer Medicare Advantage over their group plan.
The education process often starts with group insurance seminars. “We will provide an education session to an employer group, and six months later we will get a call and someone says, ‘I’m going to retire now. Can you help me?’” Miklos says. “We are farming and planting the seeds by doing those employer sessions. They now have someone to turn to and to help with the transition process.”
This was part of the thought process behind InsureOne Benefits’ affiliation with Oswald, Miklos says. “Our affiliation with Oswald provides us with the opportunity to be an additional asset to their current risk management planning and benefit services departments,” Miklos says. “One example would be working closely with Oswald Financial, who are instrumental in helping people plan for retirement. This provides us with an opportunity to play a key part in their financial future. One of the biggest concerns for planning for your retirement is your healthcare costs. We now fill that void and are here to assist in finding plans that meet both their medical and financial needs.”
Translating Is Key
For Medicare Advantage, brokers and agents face a vast array of certification requirements, such as courses from America’s Health Insurance Plans on Medicare products, plus additional courses that carriers require to represent their products. “I know brokers who have chosen not to deal with Medicare Advantage certification, and thus they only can sell Medicare Supplement, not Medicare D or Medicare Advantage, which require certification,” Gavino says. “That means they are only giving the client one third of the options, which is not right.”
Comparing Medicare Advantage offerings is made easier by federal search engines offered at Medicare.gov, which allows one to search for Medicare Advantage plans within different regions. While a consumer theoretically could just use the engines themselves and choose, Adelberg says, many will rely upon brokers and agents to perform that critical analysis.
“For the percentage of Medicare beneficiaries who are comfortable going to a government website and know enough about insurance terminology, using the government website is a good option,” he says. “It is a bit like a consumer who bypasses a traditional travel agent and goes to Expedia to buy travel tickets. But the stakes are a lot higher for a sick person or a person with expensive medical conditions. For many, the best options may not be as clear. For example, one plan might have a $10 co-pay and a 25% co-insurance, and another might have a $25 co-pay and a 10% co-insurance. The average consumer may not know which is the better deal, but for those who know insurance, it is obvious which is the better deal.”
Keeping track of the details of individual plans can present a lot of work for brokers and agents. In markets with vast pools of retirees, like California or South Florida, brokers and agents might need to keep track of the terms and value propositions of 10 different insurers. “Given each of those insurers might have 10 different plans,” Adelberg says, “there could be 100 competing plans from 10 companies.”




