In the second of a two-part series, Leader’s Edge sat down with the Claros Analytics team: Todd Owen, President & CEO; Gary Miller, Head Actuary; and Dan Wolsk, Chief Revenue Officer. They talked 2021 budget conversations, the pros and cons of claims data, and why it’s a good time to consider a self-funded approach.
Wolsk: At a national level we are starting to see insurers report Q2 financials. UnitedHealthcare reported record profits for Q2, and Anthem reported exactly the same thing. The reason is that utilization in April was down 40%. That tells us that the fully insured carriers are doing quite well during this period. We’ve heard anecdotally efforts being made to rebate those fully insured groups, but they aren’t significant enough to affect the carriers’ profits. On the other hand, everyone who is self-insured has seen costs go down dramatically.
Miller: What Dan is saying is that if you’re fully insured, you’re paying the same premium rates, whereas the self-funded groups would actually realize a surplus, in the same way that the insurance carriers have experienced a windfall.
Owen: We’re not going out and saying we expect there to be a 40% drop in utilization on an ongoing basis, but the advantages of being self-insured are a greater degree of control over plan structure, more control in how the plan is administered, but also the financial control.
Miller: Let’s say we went through another shelter in place. If you’re self-funded, you have more control over the claims. We learned a lot from the first round [of claims we saw earlier this year]. You could have an outreach [strategy] to make sure people who have conditions aren’t ignoring them—if they need services, to get them. It’s a much better opportunity to manage your population’s health. In a full-insured environment, you would pay the carrier to do all of that.
Owen: There’s another dimension to this as well. If employees or their families have chronic conditions, that has an impact on overall cost, but that also has impact on wellness and productivity. It’s about having an effective organization and effective members within it. Employees have to feel like their employer has their interests at heart; there’s going to be a sense of loyalty and an alignment with the employer. This benefits the employer as they’re proactively helping their employees to maintain their health.
If those individuals leaving the employer-sponsored system are not seeking coverage in the individual market, some may be eligible for Medicaid or Medicare. There are cost-shifting possibilities there. Those public programs dictate trend—there’s also a selection issue with COBRA, and obviously it’s very expensive. Anyone who remains on COBRA typically needs it. From the employer group’s perspective, it tends to raise average costs. If you have a subset of individuals leave the employer-sponsored system, you could have good risks leave and do something else, including not getting coverage at all. That leads to uncompensated care—that could definitely impact costs. Hospitals that can’t collect bills have to shift the costs to the rest of us.
Wolsk: On a related point, reduction in utilization has had dramatically negative impacts on the provider sector. We’re prepared for there to be upward pressure on negotiated rates as these providers try to financially re-balance themselves. If there’s an increase in enrollment in the government-funded programs or uninsured patients who end up requiring care they can’t pay for, all of this is creating financial pressures on providers that they may then seek to get higher reimbursement from their commercial populations.
We also recommend having a tracking system where you can look at utilization and average cost per service. That will help to see when it crosses over to become hyper-normal utilization.
It also allows the broker, consultant, or advisor to think through all of the variables that could impact a group or budget, such as the average age of the population and how many people left the population and aren’t returning to work.
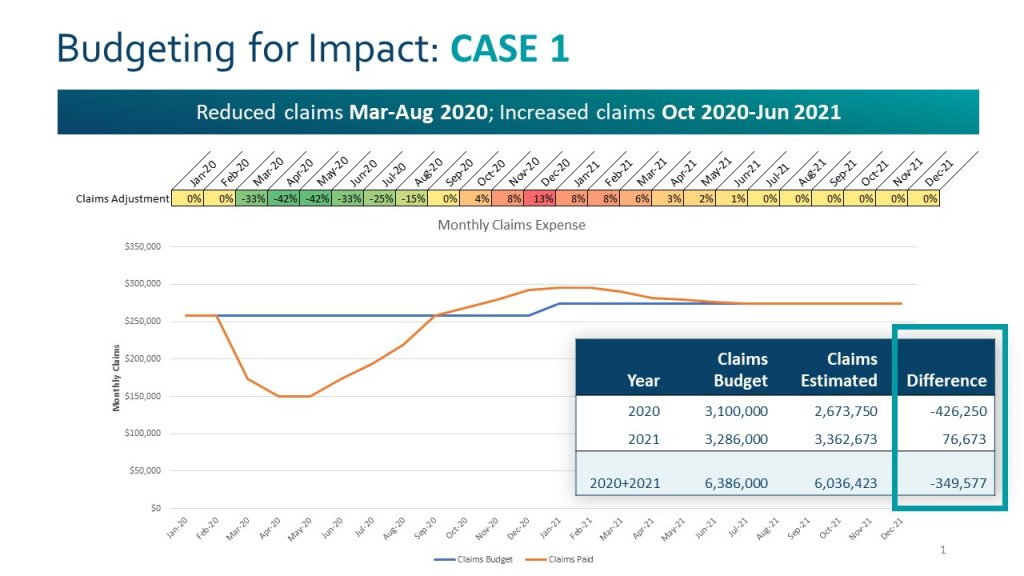
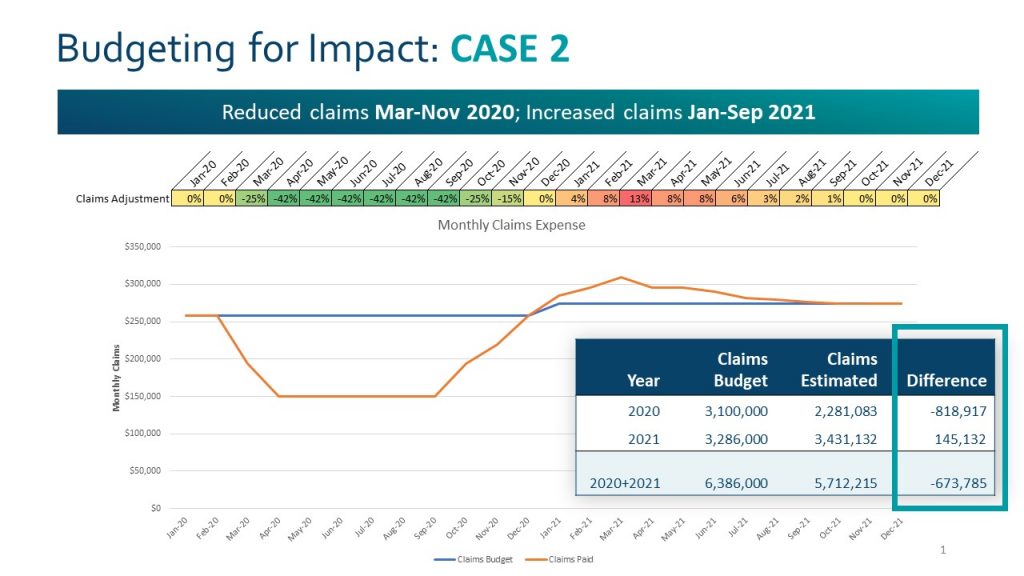
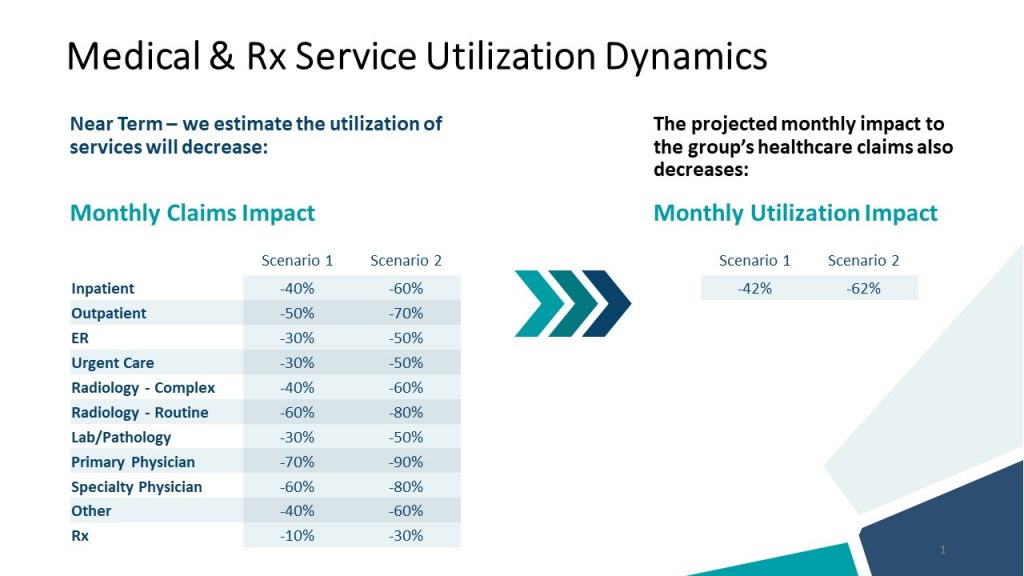
Owen: The projected decline of utilization [pictured above] is a function of COVID. We’re able to look at a range of scenarios and model the impact of changes in utilization depending on the service category. Scenarios range from low to high based on the budgeted claims for the year. We can also play with the period over which we expect to see an impact based on the depressed and elevated utilization.
Wolsk: There’s a common thread in this conversation: what we’ve seen are dramatic changes to factors in these calculations that, in the past, have been stable and predictable, and [are now] uncertain. Group sizes are changing, and utilization patterns are unpredictable. We’re suggesting that having access to your claims data gives you dramatically better insight, but we’re also saying that relying on past claims is not a particularly good approach to forecasting right now. There’s a paradox. The predictability that we’ve become accustomed to seeing is absent during this time. You need to tease out these factors in order to model a “what-if” scenario, accepting that we don’t yet know when utilization will rebound.
Coming around to the professional piece of this: when we think about health benefits, I want to highlight claims analytics. We predict costs by doing prospective modeling. However, in addition to that, there’s a lot of value in having a window into the claims data to understand how to identify those in the population who are more at risk. Understanding how members are engaging with the health plan and utilizing the services offered allows [brokers] to be proactive with what they learn from the data.